Laminitis is an extremely painful condition affecting the feet of horses (picture 1). The term laminitis refers to inflammation of the laminae. When inflamed the laminae become painful and swollen and their ability to suspend the pedal bone within the hoof capsule becomes compromised, which can result in sinking and rotation of the pedal bone (picture 2). In severe cases the pedal bone may end up prolapsing through the sole of the foot. Considering this, it is no wonder that laminitis is one of the most painful conditions that a horse or pony can suffer from. As such all cases of laminitis constitute a veterinary emergency.
Laminitis may be caused by:
|
Picture 1: Pony Exhibiting classic laminitic stance |
Picture 2: X-ray of a laminitic foot (note rotation and re-modeling of the pedal bone) |
Generally, treatment of acute laminitis relies on box rest, anti-inflammatory and pain relieving drugs, such as phenylbutazone (bute), and adequate support of the feet either through specially designed frog supports or deep bedding.
It is usually recommended that radiographs (X-rays) are taken as part of the laminitis investigation. This provides valuable information about any rotation and sinking of the pedal bone, which may have occurred. Subsequently, it can give valuable prognostic information. Radiographs also help the farrier to correctly trim the foot to try to re-align the pedal bone with the hoof wall capsule. Often it is necessary to take repeat X-rays several weeks or months later, to aid with corrective farriery.
As well as radiographs, once the horse has recovered from the acute (sore) phase, veterinary investigation should be aimed at trying to identifying the underlying cause of the laminitis.
Although there are various causes of laminitis, traditionally it has always been thought that laminitis is caused by rich, lush Spring grass. This is referred to as pasture associated laminitis (PAL). However, if rich grass is the cause of laminitis, then why do some “laminitis prone” horses get laminitis even when their grazing is restricted as well as at other times of the year? We also need to consider why most horses can graze happily without getting laminitis.
It is estimated that roughly half of the PAL cases seen are caused by EMS (Equine Metabolic Syndrome) and the other half are caused by Cushing’s Disease. The relative risk depends on the age, body condition score, breed of horse and time of year. Generally, Cushing’s Disease tends to affect older, thinner looking horses, and EMS tends to affect younger, fatter native breed horses. However, it is not always as simple as this and diagnostic blood tests are required to confirm a diagnosis of either Cushing’s Disease or EMS.
Currently the exact mechanism by which these hormonal conditions are responsible for laminitis is unknown, but it is thought that excessive amounts of the hormone insulin are likely to be involved. However, further research is required to fully understand the exact mechanisms by which insulin causes laminitis.
Cushing’s Disease
Overview
Pituitary Pars Intermedia Dysfunction (PPID; Cushing’s Disease) is a common Neuroedocrinopathy (hormonal condition) affecting horses and ponies older than 15 years old. PPID results from a loss of hormonal dopamine inhibition of the pars intermedia (PI) of the pituitary gland associated with enlargement or the formation of a benign tumour of the pars intermedia (PI) of the pituitary gland. The abnormal cells of the PI (melanotropes) produce excessive amounts of pro-opiomelanocortin (POMC) and a number of POMC-derived peptide hormones including immunoreactive adrenocoticotrophin (ACTH) peptides. Clinical signs associated with PPID include hirsutism (hairiness), hypertrichosis (long hair retention), sweating, laminitis, increased thirst, increased urination, muscle wastage, lethargy, depression, recurrent infections, abnormal, localised fat distribution and occasionally neurological deficits. Evidence of these clinical signs should prompt you to contact your vet for investigation of Cushing’s Disease.
Diagnosis
 For investigating Cushing’s Disease a blood test is taken which assesses the levels of the hormone adrenocoticotrophin (ACTH). This test is known as a Basal Plasma ACTH test. This test is both a sensitive and specific test for diagnosing Cushing’s Disease and currently is the best test available.
For investigating Cushing’s Disease a blood test is taken which assesses the levels of the hormone adrenocoticotrophin (ACTH). This test is known as a Basal Plasma ACTH test. This test is both a sensitive and specific test for diagnosing Cushing’s Disease and currently is the best test available.
Seasonal variation in pituitary gland secretion activity, associated with decreasing day length can influence basal plasma ACTH levels. As such two reference values are used depending on the time of year: From August – October a range of 0-47 pg/ml are used and between November – July a range of 0-29 pg/ml.
Occasionally, Cushing’s Disease may be suspected, but the basic basal plasma ACTH results give a border-line result meaning that it is difficult to definitively diagnose Cushing’s Disease. If this is the case your vet may suggest performing a dynamic test. Probably the best dynamic test is a thyrotropin releasing hormone (TRH) stimulation test. This involves collecting a plasma sample for ACTH. Then 1 mg TRH is injected intravenously. A second sample is collected 30 minutes later for plasma ACTH. Cushing’s Disease is indicated by either a baseline plasma ACTH value greater than the seasonally adjusted reference range (typically >29 pg/ml) and/or a post stimulation plasma ACTH >100 pg/ml.
Plasma insulin concentration can be elevated in horses suffering from Cushing’s Disease, indicating a degree of insulin resistance and hyperinsulinaemia. As hyperinsulinaemia has been shown to be a predictive indicator for the development of laminitis it may have been helpful in alerting the owner as to the likelihood of laminitis developing.
Treatment
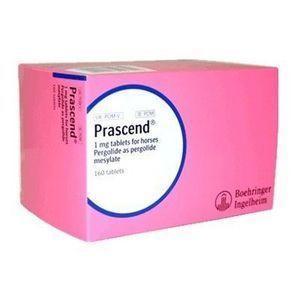 The only licensed product for the treatment of Cushing’s Disease in the horse, is the dopamine agonist Pergolide Mesylate (Prascend), which should initially be used at a dose of 2μg/kg/day orally which equates to 1 x 1mg tablet per day per 500kg horse.
The only licensed product for the treatment of Cushing’s Disease in the horse, is the dopamine agonist Pergolide Mesylate (Prascend), which should initially be used at a dose of 2μg/kg/day orally which equates to 1 x 1mg tablet per day per 500kg horse.
Repeat examination and blood sampling should be performed in around 4 weeks time to assess response to treatment, and then every 6 months to ensure that adequate treatment continues. If an inadequate response to treatment is noted, which may occur as the pony ages, then the dose of pergolide can be gradually increased by 1-2μg/kg increments up to a total of 10μg/kg (5 times the original dose). Pergolide is a very safe treatment for Cushing’s Disease.
As well as using Pergolide tablets to manage the condition it is important to remember that horses suffering from Cushing’s Disease are more prone to infections, and as such, they should have regular preventative health care such as vaccinations and dental treatment.
Equine Metabolic Syndrome (EMS)
Overview
EMS is similar to Type II Diabetes in humans. Similar to humans, the clinical signs of EMS in horses and ponies are:
Native British ponies are at the greatest risk of developing EMS, but the condition is also seen in many other horse breeds. Most cases of laminitis in horses and ponies with EMS are seen in the Spring. This is because when they ingest grass with higher than normal levels of sugar, it results in higher levels of circulating glucose and insulin. This exacerbates their existing insulin resistance and therefore increases their risk of laminitis. However, remember that grazing on its own is unlikely to cause laminitis if there is not an underlying hormonal problem. In these cases it is likely that the grass acts as the trigger factor, causing excessive release of insulin, in these insulin resistant animals.
It is important to note that many horses and ponies have both Cushing’s Disease and EMS and therefore it is important that these animals should be tested for the presence of both diseases.
Diagnosis
When trying to diagnose EMS it is important to get as much historical information about the horse or pony being examined as possible. The medical history can be very suggestive of EMS being the cause of laminitis. Historical factors to consider are:
The clinical examination can also be highly suggestive of EMS. Clinical signs to consider are:

Picture 5: Obese pony - a risk candidate for EMS
Although the history and clinical signs are often highly suggestive of EMS, diagnostic laboratory tests should be used to confirm the clinical suspicion of EMS. These include both basal and dynamic tests:
Basal tests
Dynamic tests
Treatment/Management
Management of EMS really relies on lifestyle changes, i.e. dietary modification and exercise. In more stubborn cases, medical treatment may also be included in the management regimen.
Management changes
Weight reduction – dietary modification
Exercise
Medical management
To find out more about laminitis or to discuss an investigation for your horse, please contact Central Equine Vets on 0131 664 5606